
Impact of Climate Change on Metabolic Disorders
Mitigation measures and key take home messages.
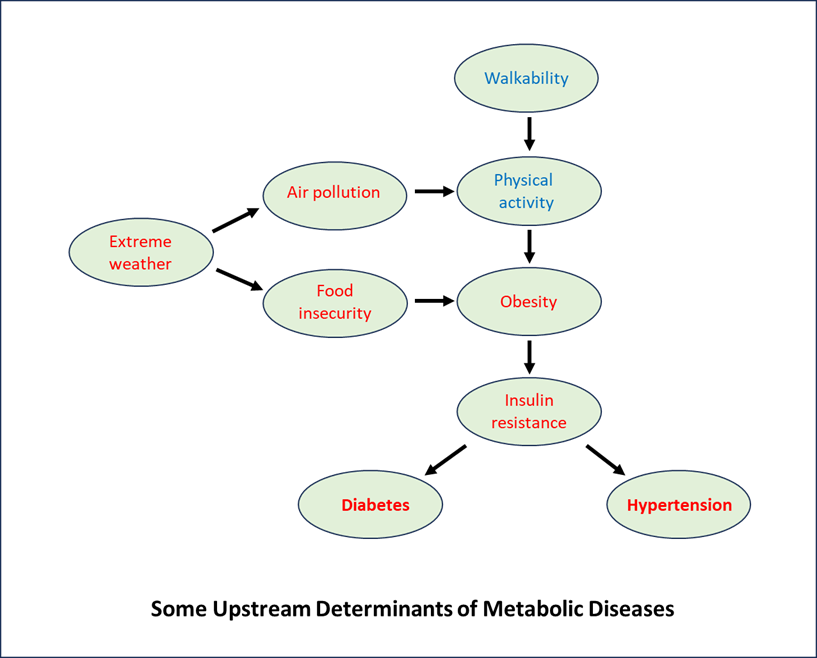
The possible mitigation
measures for climate change effects on metabolic disorders can be envisaged by
considering the upstream determinants of diseases such as diabetes:
Mitigation measures could
include:
Ø
Increased walkability and active travel. More distances
walked and cycled by individuals, and reduced air pollution levels could be achieved
with well planned urban environments, through transport policies and urban
design.
Ø Food policies that encourage shifting
the diet from a highly processed and animal-based diet to a ‘sustainable diet’ that offers low environmental
impacts, delivers food and nutrition security, and supports a healthy lifestyle
for present and future generations. To ensure sustainable diets, sustainable
food systems coupled with sustainable agriculture are required.
Ø At national level, a multisectoral approach will be
needed to develop a strategy for geo-environmental
diabetes management. In regions at risk for geological or extreme
weather events there is a need for coordinated efforts of the government, NGOs,
and healthcare institutions to:
1. Develop, implement, and disseminate preparedness plans with
targeted information for diabetes patients;
2. Develop contingency planning for emergency transport of the
most susceptible patients and actions in case of potential barriers to
accessing care;
3. Anticipate the quantity of supplies and medications for
patients;
4. Mitigate disparities in diabetes disaster preparedness.
Ø At healthcare provider level, GPs
should:
1. Identify T2D patients with cardiovascular complication or
chronic kidney disease, who may require a certain individualized management
plan;
2. Routinely conduct pre-summer medical assessment and
counselling relevant to heat exposure for people with diabetes;
3. Be aware of the potential side effects of the medicines
prescribed and adjusting dosage if necessary;
4. Conduct more frequent monitoring and check-ups during extreme
weather;
5. Implement measures to ensure that vulnerable T2D patients
stay indoors and have access to cooling systems safely during extreme heat
periods;
6. Make preparedness plans for medication and support for
climatic disasters.
Ø At patient level, individuals should:
1. Be familiar with guidelines for
disaster preparedness tailored for them;
2. Prepare a personal diabetes
emergency plan and supply kit, during and after an emergency to maintain
daily diabetes management and to help prevent acute health problems.
Ø Certain technologies could also be of great importance
in geo-environmental diabetes management:
1. Geographic information systems for mapping urban areas with increased patient vulnerability
to heat;
2. Wireless transmission of personal
blood glucose data by patients to a centralized electronic health record system
for early detection of epidemic disease outbreaks;
3. Centrally monitoring individual glucose control
during extreme weather for early intervention (e.g. a phone
call to the patient to provide advice on whether to seek medical attention);
4. Real-time methods (e.g., transmission of mobile text messages
by local area weather services) for communication
of weather advisories to patients with diabetes.
Key take home messages:
Ø
The climate crisis and
diabetes/ obesity pandemics are interconnected health issues which have common
predisposing vectors and magnify each other's impacts.
Ø
The three shared common global
vectors are increased urbanisation, increased reliance on mechanized
transportation and increased production and consumption of meat and
ultra-processed foods.
Ø
Both crises have shared common
solutions - public health actions for lifestyle changes and sustainable
urbanisation.
Ø
Health professionals should
guide a joint action on tackling climate - health issues